Many years ago as a probationary ambulance officer. I attended my first stroke victim. He was an elderly gent that had never really been ill before, so his presentation alarmed his wife to the point that she called for an ambulance. Not that his presentation was too bad. To paint a picture, he and his wife were doing the washing up after dinner when he tried to ask for another plate …and nothing came out except for a husky breath. He had no speech, no other signs and symptoms he just couldn’t speak. We arrived and assessed him, checked his blood sugar level to make sure that he wasn’t too low (low blood sugar can have various effects), provided our basic care and whisked him to an appropriate hospital.
There are a couple of points to this story.
- Strokes don’t always manifest in the “classic” way of a loss of strength down one side.
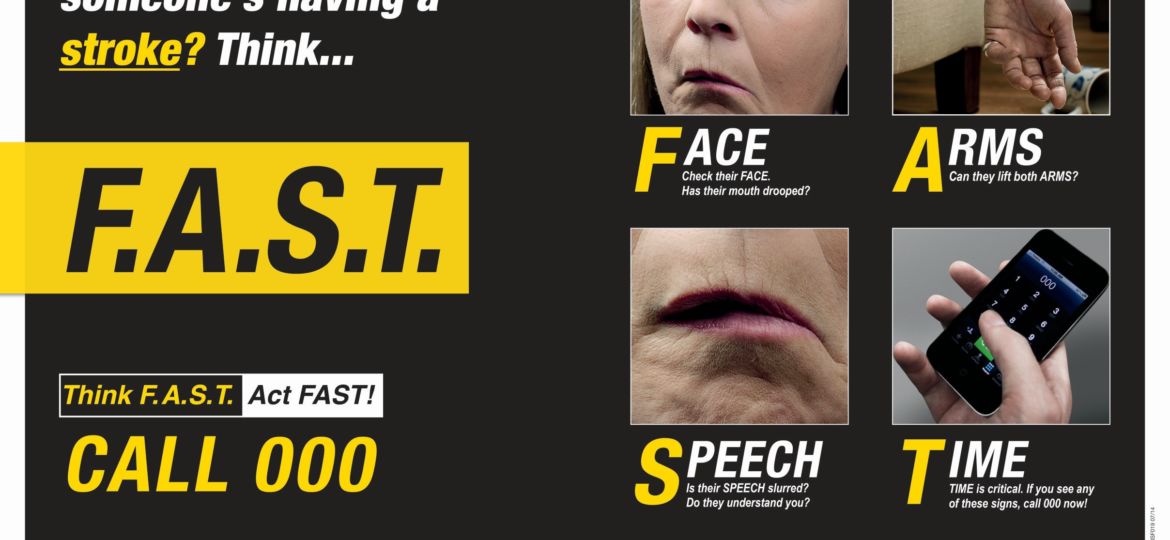
- The FAST assessment is a great way to assess whether a person has had a Stroke
Even though we didn’t have this formal assessment in those days, we assessed the same things and the outcome was a stroke victim rapidly assessed and transported to an appropriate facility
Here’s the FAST Test. Please try to remember it as it can make a difference.
F for face
Look at the persons face. Is there any abnormal drooping on one side of the face?
A for arms
As the person to raise their arms above their head at the same time. Do they have difficulty doing this? Is one arm weaker than the other?
S for speech
As the person a couple of questions. Do they appear to have difficulty speaking? Are they slurring their words?
T for time
If the person has any of the signs or symptoms listed above then it is time to call 000.
From here you would assess the level of pain the person is experiencing. The best way to do this is by using the acronym PQRST.
P for provoking factors
Question: Jerry, what were you doing when the pain came on?
It is important to know what the patient was doing at the time they experienced pain. Was Jerry walking, running, sitting, engaged in a stressful activity. Did the pain come on from a muscular activity like lifting or carrying something? Remember we are trying to ascertain the cause of the pain all the while assuming that it is cardiac in origin until ruled out.
Q for Quality
Question: Jerry what does the pain feel like?
This question will give an indication that the pain is heavy, sharp, burning, tight, squeezing, dull etc.
R for region and radiation
Question: Jerry where is the pain? Followed by does the pain go anywhere?
We need to know the origin of the pain and if it goes anywhere.
Let’s assume now that Jerry has indicated that the pain he is experiencing is heavy, starting in the centre of his chest and moving into his left jaw and arm. I’m sure by now you are getting a picture of what is possibly cardiac chest pain. What else do we need to know?
S for severity
Question: Jerry how bad is the pain? Give me a score from 0 to 10, with 0 being no pain and 10 being the worst pain you could imagine.
Pain is always subjective so you may think this has little use. My 8/10 pain may be your 2/10 pain because I have less tolerance so why is this of use at all? It will give an indication of their discomfort sure but it will also help to develop a trend over time. Once we start to give any treatment we will want to know if it is effective or not and to see if Jerry is deteriorating so while the pain scale may be a bit hit and miss, it will help show a trend.
T for time of onset
Question: What time did this happen Jerry?
Jerry may say that he has had the pain for days but it just got worse or it came on suddenly but we need to know when it started.
What have we got so far?
Jerry is a 60 yr old male that was sitting at his desk at 11am when he started to experience 6/10 heavy, central chest pain radiating to his left jaw and arm. This sounds cardiac in origin to me.
What else would we do besides calling the ambulance. Perhaps Jerry has medications that he normally takes, so we could ask about that. Perhaps ask Jerry to take a deep breath. It may sound odd considering we are pretty sure the pain is cardiac in origin, but the question has 2 uses. 1. Can Jerry actually take a deep breath or is he short of breath and 2. It he takes a deep breath and the pain is suddenly sharp and he can point to its origin with one finger perhaps we are looking at possibly a more respiratory cause. It’s just a rule of thumb and really as a first aider we only have to go so far but these sort of easy questions divide the good first aiders from the rest.
So there you have it, PQRST of pain is a great way to help remember some of the basics when it comes to assessment of someone with pain in the chest. There are other things that we can do too but we’ll leave that for another time.
Written by
Steve Riley